|
Common Eye Conditions
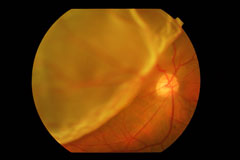
Retinal Detachment
|
The retina is the layer of nerve cells at the back of the interior of the eye which sends visual information to the brain via the optic nerve. It is attached in front to the vitreous body which fills the cavity of the eyeball behind the lens. At the back, the retina is attached to the choroid which contains blood vessels that supply the retina with oxygen and nutrients. |
A retinal detachment occurs when the retina separates from the choroid. This is a medical emergency as it leads to visual impairment and possible blindness, if not treated in time.
Causes
Retinal tears or holes are the commonest cause of retinal detachment.
These result when the vitreous body shrinks and pulls on the retina, which then breaks, allowing liquid from the vitreous gel to flow into and accumulate in the space between the retina and the choroid. This is known as posterior vitreous detachment and can occur spontaneously as part of the aging process.
As the liquid collects, the retina ‘peels away’ from the underlying choroids, resulting in a retinal detachment. The areas where it is separated lose their ability to perceive light, thus affecting vision.
Risk factors for developing tears/ holes include:
- High myopia
- Diabetes
- Cataract surgery
- Eye conditions eg uveitis, tumours
- Eye injury
- Heredity
Symptoms
Retinal detachment is painless but warning symptoms almost always appear before it occurs. These include:
- Seeing a sudden increase of many floaters
- Seeing light flashes
- Seeing a shadow or ‘curtain’ over part of the visual field
- Sudden blurred or total loss of vision
Any of these should prompt an urgent evaluation by an eye doctor to save and preserve vision.
Treatment
Surgery is the only effective treatment for retinal tears, holes and detachment. Early intervention to repair tears and holes before the retina has detached or before the central part (macula) of the retina is affected has the best chances of preserving sight.
Surgery for retinal tears
Laser photocoagulation
A laser beam is directed into the eye through a special contact lens or ophthalmoscope to make ‘burns’ around the retinal tear. These cause scarring around the tear which then ‘welds’ the retina to the underlying tissue.No incision is needed and it causes less irritation than cryopexy.
Cryopexy
This procedure is suitable for tears which are not easily accessible to the laser ( eg around the retinal periphery ) and uses intense cold to freeze the retina around the tear. A freezing probe is applied to the outer surface of the eye over the retinal defect. This causes a delicate scar which then helps secure the retina to the eye wall.
Surgery for retinal detachment
- Pneumatic retinopexy
- Scleral buckling
- Vitrectomy
The type, size and location of the retinal detachment will determine which of these procedures is most suitable. Often done in conjunction with laser photocoagulation or cryopexy, the aims are to close up any retinal holes and to reduce the tug on the retina from a shrinking vitreous.
Pneumatic retinopexy
This procedure is used for an uncomplicated retinal detachment when the tear is located in the upper half of the retina. Cryopexy is initially carried out to seal the tear, after which the eye is ‘softened’ by withdrawing some fluid from between the cornea and iris. A gas bubble is then introduced into the vitreous cavity; this expands over the course of the next few days, pushing against the tear and the detached area around it. This stops the fluid flowing through the retinal tear and allows the retina to gradually reattach itself to the back wall of the eye.
Scleral buckling
This is the most common surgery for repairing a retinal detachment, usually done in an operating room under local or general anaesthesia.
The surgeon first treats any retinal holes or tears with cryopexy. A tiny silicone band ( buckle ) is then attached to the sclera of the eye over the affected area. The buckle closes the tear and helps reduce traction on the retina, which prevents further vitreous pulling and separation and allows the retina to reattach to the underlying tissue.
If there are several tears or holes or a more extensive detachment, the surgeon may create an encircling buckle around the entire circumference of the eye.
Vitrectomy
This procedure is carried out under the following circumstances:
- when bleeding or inflammation clouds the vitreous and blocks the surgeon’s view of the detached retina
- when scar tissue in the retina makes it difficult to treat the detachment by pneumatic retinopexy or scleral buckling alone
The clouded or scarred vitreous then has to be removed surgically, through a delicate incision in the sclera of the eye.
Scleral buckling may then be performed after this and the surgeon may also fill the inside of the eye with air, gas or silicone oil to help seal the retina against the wall of the eye.
Complications of Surgery
Symptoms such as discomfort, watering, swelling, redness and itching of the eyes are all common and may persist for some time after surgery. These can be treated with medicated eyedrops.
Blurred vision and double vision may also occur.
Other complications include glaucoma, cataract, vitreous bleeding and infection.
Prognosis
Over 90% of retinal detachments can be reattached by these surgical techniques. However, on occasion, more than one operation may be required. The degree of vision that returns is dependent on a number of factors and the presence of complications. As such, close monitoring by the eye surgeon is necessary for the best possible outcome.
Common Eye Conditions
- Age Related Macular Degeneration
- Blepharitis
- Cataracts
- Central Serous Chorioretinopathy
- Contact Lens Problems
- Diabetes and the Eye
- Dry Eyes
- Floaters and Flashes
- Glaucoma
- LASIK Surgery
- Pterygium and Pingueculae
- Refractive Errors
- Retinal Detachment
- Retinal Vascular Disorders
- Uveitis and Ocular Inflammations
- Vision Problems in Children