|
Common Eye Conditions
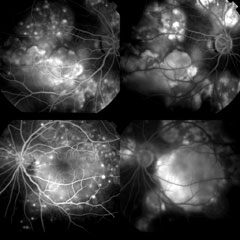
Uveitis and Ocular Inflammations
|
The eyeball consists of three layers of tissue enclosing the gel-filled vitreous cavity. These are:
Uveitis refers to inflammation of the uvea, the pigmented middle layer that contains structures responsible for the flow of blood and nutrients to the eye. This condition commonly affects people between 20 to 50 years of age and early detection and treatment will help to preserve vision better. |
Causes
- Trauma to the eye
- Viral infection eg herpes, shingles, mumps
- Bacterial infection eg syphilis
- Fungal infection eg histoplasmosis
- Generalized inflammatory disesase eg juvenile rheumatoid arthritis,
- Heredity
Types & Symptoms
Uveitis can be classified according to portion of the uvea that is affected and the symptoms will vary accordingly, although blurred vision and pain are common to all.
Anterior uveitis, affecting the iris, the front of the uvea (iritis)
Symptoms include light sensitivity, tearing, small pupil and redness around the iris. Pain is usually intense due to an increase in intraocular pressure.Intermediate uveitis, affecting the ciliary body, vitreous and retina (cyclitis)
Symptoms include sudden onset of floaters and pain may not be presentPosterior uveitis, affecting the choroid and optic nerve at the back of the eye (choroiditis/ retinitis)
Blurred vision is usually the only symptom and pain if the optic nerve is involved.Diffuse uveitis, affecting all portions of the uvea.
A combination of all the above-mentioned symptoms.
Diagnosis
Uveitis is diagnosed by the eye doctor, using slit-lamp microscopy and ophthalmoscopy. Evaluation of visual acuity and measurement of intraocular pressure are also important. Blood tests and other investigations may also be carried out to find out the underlying causes.
Treatment
Topical eyedrops and /or oral medications are usually needed to reduce inflammation and increased intraocular pressure when present. In severe cases, injections may also be necessary.
Complications
After the inflammation has subsided, the following complications may occur in the eye:
- scarring
- cataract
- glaucoma
- formation of new blood vessels
These will have to be treated accordingly with lasers, surgery and medications.
Common Eye Conditions
- Age Related Macular Degeneration
- Blepharitis
- Cataracts
- Central Serous Chorioretinopathy
- Contact Lens Problems
- Diabetes and the Eye
- Dry Eyes
- Floaters and Flashes
- Glaucoma
- LASIK Surgery
- Pterygium and Pingueculae
- Refractive Errors
- Retinal Detachment
- Retinal Vascular Disorders
- Uveitis and Ocular Inflammations
- Vision Problems in Children