|
Common Eye Conditions
Diabetes and the Eye
|
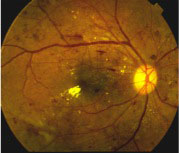
Diabetes mellitus is one of the leading causes of blindness in developed countries in the world, including Singapore. It is responsible for a spectrum of eye complications, of which the most serious is diabetic retinopathy. In this condition, the high blood sugar levels in diabetes cause changes in the retina, the light-sensitive layer of nerve cells at the back of the eye, thus leading to visual loss. There are three stages in diabetic retinopathy: |
Background retinopathy
This is the early stage in which the small blood vessels in the retina are blocked or damaged, causing swelling and leakage of blood and fluid into the vitreous body of the eye. There are usually no symptoms at this stage.
Maculopathy
The macula is the pinhead-sized central area of the retina that lets us see details. When it swells up (edema) in the background stage, central vision is gradually lost, resulting in difficulty with tasks like reading and driving.
Proliferative retinopathy
This is the advanced stage where new blood vessels form (proliferate) on the retina and optic nerve, as part of the body’s way of repairing the damage in the early stages. These new vessels are however, weak and tend to rupture, causing scarring which in turn, pulls on the retina, leading to retinal detachment ( see section on this condition ) and loss of vision.
Symptoms of Diabetic Retinopathy
- Blurred vision
- Difficulty reading or seeing details
- Seeing floaters/flashes
- Sudden loss of vision in one or both eyes
- Changes in vision throughout the day
Management of Diabetic Retinopathy
Screening
The key to successful management of diabetic retinopathy lies in screening and early detection of the changes mentioned above to allow prompt treatment.
ALL diabetic patients should have their eyes checked at least once a year by an eye doctor, irregardless of the duration of their diabetes or whether they have any visual symptoms.
The examinations carried out are fundoscopy, fluorescein angiography and retinal photography.
Prevention
It has been shown that good control of blood sugar levels and blood pressure can help to reduce the incidence of diabetic retinopathy. However, the progression of changes may still occur, despite the best of efforts.
Treatment
There is no cure for diabetic retinopathy but surgical and medical treatments are available that help reduce visual loss. These are:
- Laser surgery to seal leaky blood vessels, control macular edema and stop the growth of new blood vessels. It can also be used to treat retinal detachment.
- Vitrectomy, in which the surgeon removes the bloody vitreous from the eye and replaces it with a clear solution. This enables light to pass through and restores vision.
- Injection of intraocular steroids, especially for patients who have macular edema not responding to laser treatment
- Injection of intraocular anti-vasogenic drugs. These are the latest advances in medical treatment of retinal disease and have shown promising results in the treatment of proliferative retinopathy.
Other Diabetes Related Eye Conditions
See relevant sections
Common Eye Conditions
- Age Related Macular Degeneration
- Blepharitis
- Cataracts
- Central Serous Chorioretinopathy
- Contact Lens Problems
- Diabetes and the Eye
- Dry Eyes
- Floaters and Flashes
- Glaucoma
- LASIK Surgery
- Pterygium and Pingueculae
- Refractive Errors
- Retinal Detachment
- Retinal Vascular Disorders
- Uveitis and Ocular Inflammations
- Vision Problems in Children